What is the main cause of peripheral artery disease?
Exploring the Main Causes of Peripheral Artery Disease
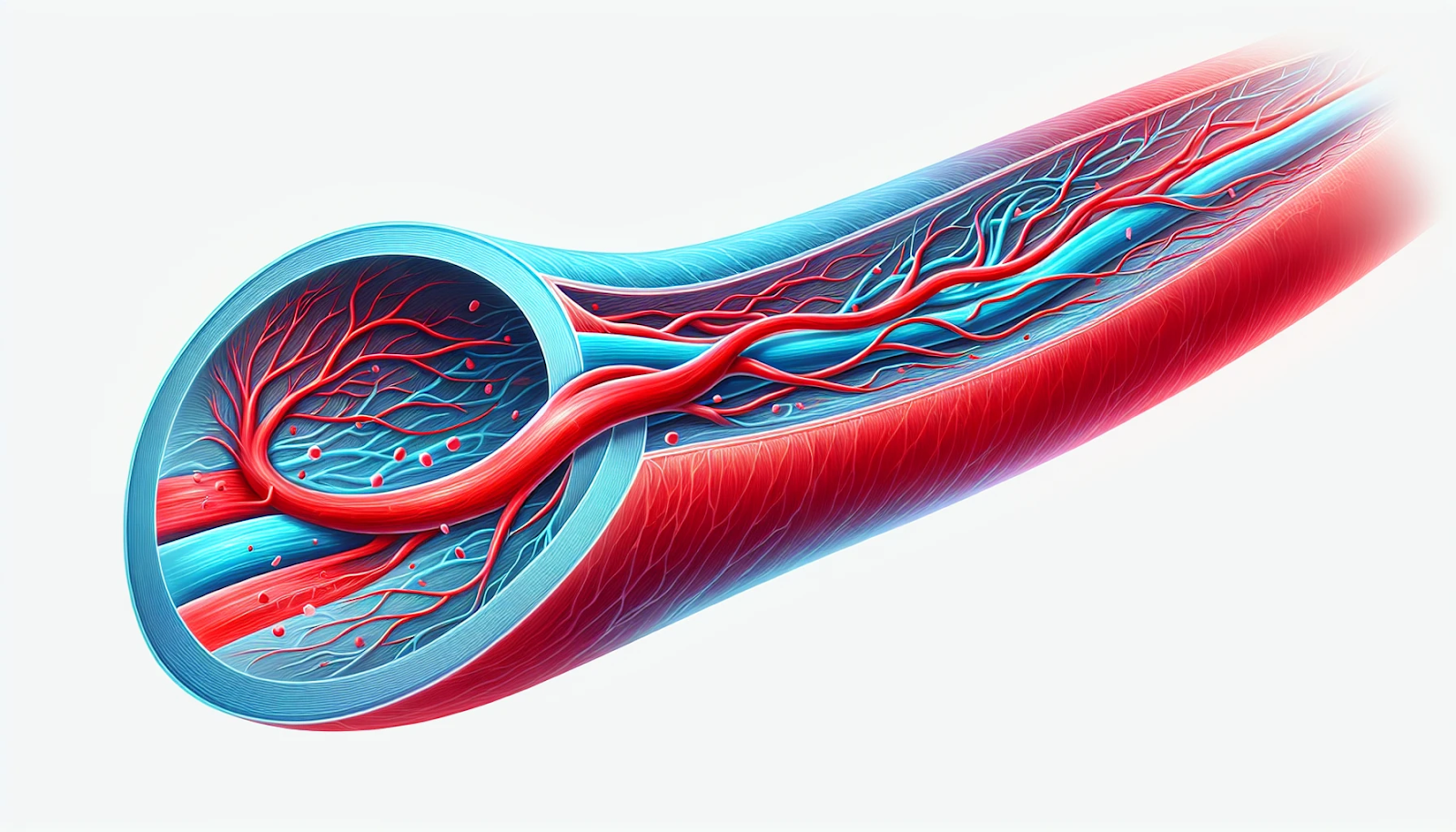
Peripheral Artery Disease (PAD) is a common circulatory problem where narrowed arteries reduce blood flow to the limbs. PAD often causes pain and fatigue, particularly in the legs during walking, and can be a sign of more widespread arterial disease. This condition can have severe consequences if left untreated, leading to limb amputation or increased risk of heart attack and stroke. This detailed exploration focuses on the primary causes, risk factors, and implications of Peripheral Artery Disease, providing vital information for understanding and managing this condition.
Understanding Peripheral Artery Disease
Peripheral Artery Disease is primarily caused by atherosclerosis, a process where fatty deposits (plaques) build up in the arterial walls, leading to reduced blood flow. While atherosclerosis is the most common cause, other conditions and factors can also contribute to the development of PAD.
Atherosclerosis: The Leading Cause
Atherosclerosis begins with damage to the artery wall, which can be triggered by various factors such as smoking, high cholesterol, high blood pressure, and high levels of sugar in the blood due to insulin resistance or diabetes. Over time, this damage leads to the accumulation of fatty substances, cholesterol, cellular waste products, calcium, and fibrin, a clotting material in the blood. These substances collectively form a plaque that narrows or blocks blood flow in the arteries.
Atherosclerosis, often known as the hardening of the arteries, is the primary cause of Peripheral Artery Disease (PAD). It involves the buildup of fats, cholesterol, and other substances in and on the artery walls (plaque), which can restrict blood flow. These plaques can burst, leading to serious cardiovascular complications. Understanding the underlying mechanisms and implications of atherosclerosis is crucial for managing and preventing PAD effectively.
The Progression of Atherosclerosis
- Initial Damage to the Arteries: This can be caused by smoking, diabetes, hypertension, and high cholesterol.
- Formation of Plaque: As the artery wall heals, it traps these materials, forming a plaque.
- Plaque Growth and Complications: Plaques can grow large enough to significantly reduce the artery’s diameter, or they can become brittle and rupture, leading to serious complications.
Other Contributing Factors
While atherosclerosis is the primary cause of PAD, several other factors can increase the risk or severity of the disease:
- Diabetes: Prolonged high blood sugar levels can damage blood vessels and hasten the atherosclerotic process.
- Smoking: Tobacco use contributes to the constriction and damage of arteries and is a major risk factor for the development and worsening of PAD.
- Hypertension: High blood pressure can cause harm to artery walls, which may speed up the narrowing caused by plaque.
- High Cholesterol: Elevated levels of bad cholesterol (low-density lipoprotein, or LDL) can contribute to plaque buildup.
- Age: The risk of PAD increases with age, particularly after 50.
- Family History: A family history of PAD, heart disease, or stroke increases your risk.
- Obesity: Excess weight typically worsens other risk factors for atherosclerosis and PAD.
The Mechanism of Atherosclerosis
Atherosclerosis is a slow, progressive disease that may start in childhood. In some people, the disease progresses rapidly in their 30s. In others, it doesn’t become threatening until they reach their 50s or 60s. Here’s a detailed look at how it develops:
1. Endothelial Injury: The process begins with damage to the endothelium, the innermost layer of the artery. Factors such as high blood pressure, turbulent blood flow, smoking, or high levels of cholesterol contribute to this damage.
2. Formation of Fatty Streaks: Once the endothelium is damaged, lipids (or fats) circulating in the blood accumulate in the arterial walls. Over time, these lipids become oxidized, causing the cells to become engorged and form what are known as fatty streaks.
3. Plaque Formation: Immune cells called macrophages consume the oxidized lipids, transforming into foam cells. These foam cells accumulate and contribute to the formation of atherosclerotic plaques. As these plaques grow, they create a bulge in the artery wall that restricts blood flow.
4. Plaque Rupture and Thrombosis: Plaques can become unstable and rupture, leading to blood clots that can further obstruct blood flow. This is a common cause of acute PAD and can result in severe vascular emergencies like heart attacks or strokes.
Risk Factors for Atherosclerosis
Several risk factors can accelerate the formation and progression of atherosclerosis, increasing the risk of developing PAD:
– High Cholesterol Levels: Excessive levels of LDL (bad) cholesterol in the blood can lead to plaque buildup.
– Smoking: Smoking damages the endothelial cells and is a major risk factor for atherosclerosis.
– High Blood Pressure: Elevated pressure in the arteries can damage the endothelium, facilitating atherosclerosis.
– Diabetes: High blood sugar levels can damage the lining of the arteries and accelerate plaque formation.
– Obesity: Excess weight typically exacerbates other risk factors, such as high blood pressure and diabetes.
– Sedentary Lifestyle: Lack of physical activity can worsen other risk factors for atherosclerosis.
Prevention and Management
Managing the risk factors for atherosclerosis can significantly reduce the likelihood of developing PAD or experiencing severe complications:
– Dietary Modifications: Eating a heart-healthy diet low in saturated fats and high in fiber can help reduce blood cholesterol levels and improve overall cardiovascular health.
– Regular Exercise: Physical activity can help maintain a healthy weight, lower cholesterol levels, and keep blood pressure in check.
– Quitting Smoking: Smoking cessation is critical for reducing the progression of atherosclerosis.
– Medication: In some cases, medications may be necessary to control cholesterol, blood pressure, or blood sugar levels.
Atherosclerosis is not just a contributing factor; it is the principal cause of Peripheral Artery Disease. Its progression from a simple endothelial injury to complex plaque formation underscores the importance of early intervention and comprehensive management strategies. By addressing the root causes and mitigating risk factors, individuals can significantly lower their risk of PAD and its potentially life-threatening complications. Regular medical check-ups, adopting a healthier lifestyle, and staying informed about cardiovascular health are essential steps in combating the impact of atherosclerosis.
Symptoms and Diagnosis of PAD
Peripheral Artery Disease (PAD) is a common yet often underdiagnosed vascular condition where the arteries that carry blood to the legs or arms are narrowed, usually due to atherosclerosis. Identifying the symptoms and getting an accurate diagnosis are critical steps in managing PAD effectively and preventing its potentially severe complications.
Recognizing the Symptoms of PAD
The symptoms of PAD can vary widely from person to person, and some individuals may not exhibit any symptoms at all (asymptomatic). However, there are several classic signs and symptoms to watch for:
- Claudication: This is the most common symptom of PAD and involves muscle pain or cramping in the legs or arms that starts during exercise and ends with rest. The pain is typically felt in the calves but can also occur in the buttocks or thighs. It’s caused by inadequate blood flow during increased demand, such as exercise.
- Numbness or Weakness: Chronic lack of blood flow can lead to feelings of numbness or weakness in the legs.
- Coldness in Lower Leg or Foot: You may notice that one leg or foot feels colder than the other, a sign of reduced blood flow.
- Change in Color of Legs: Poor circulation can cause the skin on the legs to change color, often becoming paler or bluish.
- Hair Loss or Slower Hair Growth: The legs may lose hair or grow hair more slowly than usual.
- Slower Growth of Toenails: Similarly, toenails may grow more slowly due to reduced blood supply.
- Sores on Toes, Feet, or Legs that Won’t Heal: Reduced blood flow can prevent sores or cuts from healing normally, which can increase the risk of infection or tissue death.
- Erectile Dysfunction: Men with PAD may experience erectile dysfunction, which is also related to poor blood flow.
Diagnosing Peripheral Artery Disease
Early diagnosis of PAD is crucial for effective treatment and prevention of complications. Various diagnostic tools and tests are used to confirm the presence of PAD and assess its severity:
- Physical Examination: The doctor will look for physical signs of PAD, such as weak or absent pulses in the feet or legs, cold skin, atrophic skin changes, and wounds that don’t heal.
- Ankle-Brachial Index (ABI): This simple, non-invasive test is the most common first step in diagnosing PAD. It compares the blood pressure measured at the ankle with the blood pressure measured at the arm. An ABI ratio of less than 0.90 is generally indicative of PAD.
- Doppler Ultrasound: This imaging technique visualizes blood flow and can identify blocked or narrowed arteries. It also helps determine the severity of PAD and locate specific areas of obstruction.
- Computed Tomographic Angiography (CTA) and Magnetic Resonance Angiography (MRA): These imaging tests provide detailed images of blood vessels and are useful for planning interventions.
- Angiography: While it’s more invasive, angiography is considered the gold standard for diagnosing PAD. A contrast dye is injected into the arteries, making them visible on an X-ray. This test can precisely locate blockages and assess the structure of blood vessels.
Awareness of the symptoms and understanding the diagnostic pathways are essential for managing PAD. Individuals experiencing symptoms of PAD, particularly those who have risk factors such as smoking, diabetes, high cholesterol, or a family history of vascular disease, should seek prompt medical evaluation. Early diagnosis and treatment can improve quality of life, enhance mobility, and reduce the risk of complications like limb loss or cardiovascular events. Regular check-ups and adherence to treatment plans, including lifestyle changes and medications, play a crucial role in managing the progression of PAD.
Treatment and Prevention of PAD
Peripheral Artery Disease (PAD) can significantly impact quality of life due to symptoms like pain during walking and increased risk of cardiovascular events. Effective treatment and proactive prevention are crucial in managing PAD, improving symptoms, and reducing risks of serious complications. This section details various treatment options and preventive measures for PAD.
Treatment Options for PAD
Treatment for PAD aims to manage symptoms and stop the progression of the disease. The approach often depends on the severity of the condition and the specific needs of the patient.
- Lifestyle Changes: Fundamental changes in daily habits can have a significant impact on slowing the progression of PAD and alleviating symptoms.
- Exercise: A supervised exercise program is one of the most effective treatments for PAD. Regular walking regimens prescribed by a healthcare provider can improve mobility and reduce pain.
- Diet: Adopting a heart-healthy diet low in saturated fats, rich in fruits, vegetables, and whole grains can help lower blood cholesterol levels and improve cardiovascular health.
- Quit Smoking: Smoking cessation is critical as smoking is a major risk factor for the development and progression of PAD.
- Medications:
- Cholesterol-lowering drugs: Statins are commonly prescribed to reduce cholesterol levels and stabilize plaque in the arteries.
- High blood pressure medications: Controlling blood pressure is crucial for patients with PAD.
- Medications to control blood sugar: For diabetic patients, maintaining blood sugar levels is essential in slowing the progression of PAD.
- Blood thinners: Drugs like aspirin or clopidogrel may be prescribed to prevent blood clots that can worsen PAD or lead to other vascular complications.
- Surgical Treatments:
- Angioplasty and Stenting: In this procedure, a small balloon attached to a catheter is inflated within the artery to open the blockage. A stent may be placed to keep the artery open.
- Bypass Surgery: For severe cases, a bypass grafting surgery may be performed to reroute blood flow around the blocked artery.
- Atherectomy: This is a less common procedure where the plaque is mechanically removed from the arteries.
Prevention of PAD
Preventing PAD involves addressing the risk factors that lead to its development. Here are key preventive measures:
- Cardiovascular Risk Assessment: Regular check-ups to evaluate risk factors such as cholesterol levels, blood pressure, and blood sugar levels can help catch potential problems early.
- Maintain a Healthy Lifestyle: A balanced diet and regular physical activity can greatly reduce the risk of developing PAD.
- Monitor and Manage Chronic Conditions: Effectively managing diabetes, high blood pressure, and high cholesterol is essential in preventing PAD.
- Avoid Smoking: Smoking is a major risk factor for PAD. Quitting smoking can dramatically reduce the risk of developing PAD and other cardiovascular diseases.
Education and Regular Check-ups
Educating patients about the symptoms and risks associated with PAD is crucial for early detection and treatment. Regular check-ups with a healthcare provider not only help monitor the status of the disease but also provide ongoing support for managing health effectively.
The treatment and prevention of Peripheral Artery Disease involve a combination of lifestyle changes, medications, possible surgical interventions, and regular monitoring of health status. Through proactive management and preventive measures, individuals with PAD can lead healthier lives and minimize the risk of complications. It’s important for patients to work closely with their healthcare providers to tailor a treatment plan that best fits their individual needs and to maintain diligent follow-up care.

Conclusion
Understanding the main causes of Peripheral Artery Disease is crucial for prevention and management. Lifestyle choices play a significant role in both the development and treatment of PAD. By addressing risk factors such as smoking
, diabetes, and high cholesterol, individuals can significantly reduce their chances of developing this debilitating condition. Regular check-ups and following a healthy lifestyle are vital strategies for preventing and managing PAD effectively.
DR. ALOK KUMAR UDIYA
Well-known Interventional Radiologist Dr. ALOK KUMAR UDIYA is currently a consultant at The CARE CHL, an Indore hospital with NABH accreditation. He has a distinguished medical career and has studied at numerous top federal, state, and international superspecialty medical institutes.
He earned his M.B.B.S. from M G M Medical College in Indore and then M.D. in radiodiagnosis from Lady Hardinge Medical College at Delhi University.
Following that, he completed a fellowship in neuro- and vascular interventional radiology at the Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGIMS) in Lucknow, where he gained extensive experience in diagnostic imaging along with hepatobiliary, peripheral vascular, and neurovascular interventions.
The prestigious Institute of the liver and biliary sciences Hospital (ILBS), New Delhi, awarded him a P.D.C.C. (Post Doctoral fellowship) in Hepatobiliary intervention, where he also received further in-depth instruction and advanced training in hepatobiliary and transplant imaging and interventions.
Moreover, he completed a six-month Neuro-Interventional Fellowship (FINR) at the famous University of Zurich, where he received specialized training from Professor Anton Valavanis in the endovascular management of stroke and aneurysm. https://cvicvascular.com/
Contact Us
Contact No. – 099993 78980
Email – dralokudiya@gmail.com
Hospital
Care CHL
Address – AB Rd, near L.I.G Square, RSS Nagar, Indore, Madhya Pradesh 452008
Time – 10am to 5pm
Clinic
Address – 403 Panama Tower Geeta Bhawan Square Near Crown Palace, Indore, Madhya Pradesh
Time – 6pm To 8pm
Read More –
What is the main cause of peripheral vascular disease?
https://test.mangalcart.com/main-cause-of-peripheral-vascular-disease/
How do you treat a vascular disease?
https://test.mangalcart.com/how-do-you-treat-a-vascular-disease/
Recognizing the Early Warning Signs of Gangrene: A Vital Guide
https://test.mangalcart.com/early-warning-signs-of-gangrene/
