Recognizing the Early Warning Signs of Gangrene: A Vital Guide
Introduction
Gangrene is a serious medical condition that arises when a considerable mass of body tissue dies (necrosis). This condition is mostly caused by a lack of blood supply and can lead to severe complications if not identified and treated promptly. Recognizing the early signs of gangrene can be lifesaving, enabling early medical intervention to prevent further tissue death and manage the condition effectively. This blog explores the Early Warning Signs of Gangrene, the types of gangrene, and the necessary steps to take if you suspect its presence.
Understanding Gangrene: Types and Causes
Gangrene, a serious medical condition, involves the death of body tissue due to a significant loss of blood supply. The causes and risk factors of gangrene are diverse, encompassing issues from circulatory problems to infections. Understanding the different types of gangrene and their respective causes is crucial for both prevention and effective management.

Types of Gangrene
Gangrene can be classified into several types, each with unique characteristics and underlying causes:
1. Dry Gangrene: Dry gangrene occurs when the blood supply to certain body parts, typically the extremities like toes and fingers, becomes significantly reduced. Without adequate blood, the tissue slowly dies due to a lack of oxygen and nutrients.
– Common Causes: The most frequent cause of dry gangrene is peripheral arterial disease (PAD), which narrows and blocks arteries, reducing blood flow. Other contributing factors include diabetes and frostbite.
– Appearance: The affected area often appears dry, shriveled, and dark (ranging from brown to purplish-black). This type of gangrene progresses slowly and is less likely to cause an infection because it occurs in body parts with less moisture.
2. Wet Gangrene: Wet gangrene develops when body tissue becomes infected with bacteria, leading to a sudden stoppage of blood flow. The presence of infection causes the affected tissue to die more quickly.
– Common Causes: Wet gangrene can occur after a severe burn, frostbite, or injury that becomes infected. It can also develop from an internal problem, such as a burst appendix, leading to peritonitis.
– Appearance: The affected area is usually swollen, blistered, and wet, emitting a foul odor. This type of gangrene is considered an emergency because it can spread rapidly and is life-threatening.
3. Gas Gangrene: Gas gangrene is a deadly form of wet gangrene that occurs when a specific bacteria, usually *Clostridium perfringens*, infects a wound, producing gas within the tissue.
– Common Causes: The infection typically develops in deep wounds contaminated with dirt, debris, or decaying matter, which are conducive environments for these bacteria.
– Appearance: Infected tissue might appear pale or brownish-red and can feel spongy to the touch due to gas production. Patients may also experience severe pain and swelling in the affected area.
4. Internal Gangrene: This type occurs when blood flow to an internal organ is blocked.
– Common Causes: Conditions that can lead to internal gangrene include hernias, gallstones, or twisted or pinched intestines.
– Appearance: Symptoms vary depending on the affected organ but can include severe pain and fever. This type of gangrene can be difficult to diagnose because the symptoms are internal and not visible from the outside.
5. Fournier’s Gangrene: A rare but severe type of gangrene that typically affects the male genitalia and surrounding areas.
– Common Causes: It is usually caused by a bacterial infection and often starts in the genital area, rapidly spreading to other parts of the body.
– Appearance: The area may turn black, emit a foul odor, and show signs of severe inflammation.
Causes and Risk Factors
The primary cause of gangrene is reduced blood supply, often exacerbated by one or more risk factors:
– Diabetes: High blood sugar levels can damage blood vessels, impairing circulation and increasing the risk of infections.
– Injuries: Severe injuries that damage blood vessels can lead to gangrene, particularly if the wound is not properly cared for.
– Infectious Diseases: Certain infections can cause rapid tissue death and systemic issues.
– Vascular Diseases: Conditions like atherosclerosis that narrow blood vessels and decrease blood flow can lead to gangrene.
– Immune System Problems: A weakened immune system, either from medical conditions or medications, can increase susceptibility to infections that lead to gangrene.
Understanding these types and causes is vital for both medical professionals and patients to ensure timely diagnosis and treatment, which can significantly improve outcomes in cases of gangrene.
Early Warning Signs of Gangrene
Gangrene is a serious condition that requires immediate medical attention. It occurs when tissue in the body dies due to a loss of blood supply. Early detection and treatment are critical to prevent the spread of gangrene, which can lead to amputations or even be life-threatening. Here’s a comprehensive look at the early signs of gangrene that you should be aware of:
Recognizing the Early Indicators
1. Skin Discoloration
– Key Sign: The first and often most noticeable sign of gangrene is a significant change in skin color. This can manifest as an unusual redness in the early stages, which may then progress to darker shades including blue, purple, green, black, or bronze.
– Progression: Initially, the discoloration may appear as a small spot but can quickly spread depending on the type of gangrene and the underlying cause.
2. Swelling or Edema
– Key Sign: Swelling is common in cases of wet gangrene, where the infection causes an inflammatory response. The area may feel tight, puffy, and swollen.
– Progression: As the condition worsens, the swelling can increase and become more painful.
3. Pain
– Key Sign: Pain is another early indicator, particularly when gangrene is caused by an infection or injury. The pain may start as mild but can escalate rapidly as the condition worsens.
– Progression: Surprisingly, the pain might decrease as the nerve endings in the tissue die off, which often leads to the next sign.
4. Numbness or Loss of Sensation
– Key Sign: A lack of feeling in the affected area often follows the initial episodes of pain. This loss of sensation occurs because gangrene affects the nerves.
– Progression: Numbness can be a dangerous sign, as it might lead individuals to delay seeking treatment because the pain subsides.
5. Sores or Blisters
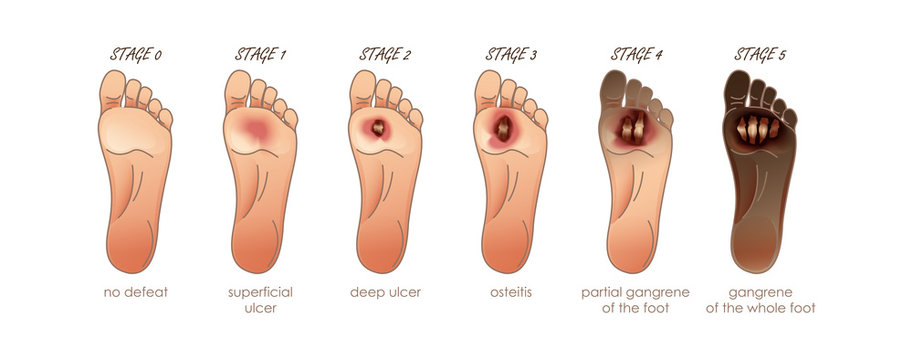
– Key Sign: Unexplained sores, blisters, or ulcers that appear on the skin and do not heal normally can be early signs of gangrene, especially in individuals with diabetes.
– Progression: These wounds can increase in size and depth, emitting a foul-smelling discharge as the tissue begins to die.
6. Foul-smelling Discharge
– Key Sign: A significant and noticeable foul odor may emanate from the affected area. This is particularly characteristic of wet gangrene, where bacterial infection is involved.
– Progression: As the infection worsens, the discharge may become more pronounced and offensive.
7. Skin Texture Changes
– Key Sign: The texture of the skin may change, becoming thin, shiny, or tight. Dry gangrene often causes the skin to look shriveled and dry.
– Progression: The affected area can eventually become completely dry and black, resembling mummified skin.
Critical Actions and Early Intervention
If you or someone you know exhibits any of these signs, especially if they have an underlying condition like diabetes or peripheral arterial disease, it is crucial to seek immediate medical care. Early stages of gangrene can often be managed more effectively if caught promptly. The course of treatment may include surgery to remove dead tissue, antibiotics to treat any infection, and measures to restore blood flow to the affected area.
Preventive measures are also important, particularly for those at higher risk. This includes regular monitoring of the feet and legs, managing diabetes effectively, quitting smoking to improve circulation, and ensuring wounds are cleaned and dressed properly to prevent infection.
Being aware of the early signs of gangrene and responding swiftly to these symptoms can significantly improve the prognosis and help prevent severe outcomes, including the loss of limbs or life-threatening complications.
Diagnosis and Treatment
Gangrene is a severe medical condition that necessitates prompt diagnosis and treatment to prevent life-threatening complications. Early recognition of symptoms is crucial, but a definitive diagnosis and subsequent treatment strategy rely on a combination of clinical assessment, imaging, and sometimes surgical intervention. Here’s an in-depth look at how gangrene is diagnosed and treated:

Diagnosis of Gangrene
1. Physical Examination
– Initial Step: A doctor will start with a thorough physical examination, assessing the discoloration, texture, and other changes in the affected area. They will look for signs of sensitivity, odor, or discharge that are indicative of gangrene.
– Importance: This step helps to determine the presence of infection and the type of gangrene, which can guide further diagnostic tests.
2. Imaging Tests
– Types of Imaging: Imaging tests such as X-rays, MRI (Magnetic Resonance Imaging), and CT (Computed Tomography) scans are used to view the affected areas in detail. These tests help to show the extent of the damage and whether the gangrene has spread to surrounding tissues or bones.
– Purpose: Imaging helps to visualize blockages in blood vessels that may have led to reduced blood flow, a common cause of gangrene.
3. Blood Tests
– Laboratory Analysis: Blood tests can check for signs of infection or sepsis (a potentially life-threatening response to infection). Elevated white blood cell counts are common indicators of infection.
– Further Testing: Other tests might include checking for diabetes and assessing kidney function, which can be affected by severe infections.
4. Tissue Biopsy
– Procedure: In some cases, a biopsy of the affected tissue may be necessary. This involves taking a small sample of the tissue and analyzing it in a lab to confirm the presence of gangrene and identify the types of bacteria or other pathogens involved.
– Confirmation: This test can confirm the diagnosis and help in formulating a targeted treatment plan.
Treatment of Gangrene
1. Surgical Intervention
– Debridement: The removal of dead tissue, or debridement, is a crucial first step in treating gangrene. This procedure helps to prevent the spread of infection and allows healthy tissue to heal more effectively.
– Amputation: In severe cases, where the gangrene is extensive and poses a threat to the patient’s life, amputation of the affected limb or part may be necessary.
2. Antibiotics
– Infection Control: If the gangrene is caused by an infection, intravenous antibiotics are typically administered to control and eliminate the infection. The type of antibiotics used depends on the specific bacteria causing the infection.
3. Hyperbaric Oxygen Therapy
– Procedure: This treatment involves placing the patient in a special chamber that increases the oxygen level in the blood. The high levels of oxygen can help heal the affected tissue, combat certain types of bacteria, and improve outcomes in patients with certain types of gangrene, particularly those with diabetes.
– Benefits: Hyperbaric oxygen therapy can be particularly effective in treating wet gangrene and enhancing the healing process.
4. Vascular Surgery
– Restoring Blood Flow: For gangrene caused by impaired blood flow, vascular surgery may be required to bypass or dilate blood vessels, thereby restoring circulation to the affected area.
– Long-term Management: This may also involve long-term management of underlying conditions such as diabetes and peripheral arterial disease to prevent recurrence.
5. Supportive Care
– Nutritional Support: Proper nutritional support is essential for healing and recovery. Patients might need a diet rich in vitamins and minerals to enhance immune function and tissue repair.
– Pain Management: Effective pain management strategies are critical, especially post-surgery, to ensure patient comfort and promote recovery.
Follow-Up and Rehabilitation
After initial treatment, rigorous follow-up is necessary to ensure that the treatment has been successful, to manage pain, and to begin rehabilitation, especially if the patient has undergone amputation. Physical therapy, along with psychological support, is crucial to help patients adjust to lifestyle changes and regain function.
The journey from diagnosis to treatment and beyond requires a multidisciplinary approach involving surgeons, infectious disease specialists, physiotherapists, and sometimes psychologists. Early diagnosis and prompt, aggressive treatment are the keys to managing gangrene effectively and reducing the risk of severe outcomes.
Prevention Tips
Preventing gangrene, a severe condition characterized by the death of body tissues, involves managing risk factors and adopting healthy lifestyle habits. Early detection and proper management of conditions that can impede blood flow are crucial. Here are essential prevention tips that can significantly lower the risk of developing gangrene:

Manage Underlying Health Conditions
1. Control Diabetes
– Monitor Blood Sugar: Regular monitoring and maintaining blood glucose levels within the recommended range are crucial. Uncontrolled diabetes can cause damage to blood vessels, impairing circulation.
– Regular Check-Ups: Routine visits to a healthcare provider for diabetes management can help prevent complications that could lead to gangrene.
2. Address Peripheral Arterial Disease (PAD)
– Lifestyle Changes: Adopting a healthy diet, exercising regularly, and managing cholesterol levels can improve blood flow and prevent the progression of PAD.
– Medication Compliance: If prescribed, medications to improve blood flow should be taken as directed.
Maintain Good Hygiene and Wound Care
1. Skin Care
– Regular Inspection: Regularly inspect feet and legs (or other at-risk areas) for cuts, bruises, or signs of infection, especially if you have sensory deficits.
– Hygiene: Keep your skin clean and moisturized to prevent cracks and dryness, which can become gateways for infection.
2. Prompt Wound Management
– Clean and Cover: Clean all minor cuts and scrapes with water and gentle soap. Cover them with a sterile bandage until they heal completely.
– Seek Medical Advice: For more significant injuries or if you notice signs of infection (redness, warmth, swelling, or pus), consult a healthcare provider promptly.
Adopt a Healthy Lifestyle
1. Nutrition
– Balanced Diet: Eat a balanced diet rich in vitamins and minerals, which can boost the immune system and promote vascular health.
– Hydration: Staying hydrated helps maintain the health of cells and circulatory system.
2. Exercise
– Regular Activity: Engage in regular physical activity to enhance blood flow and maintain general health. Even simple activities like walking can be beneficial.
3. Smoking Cessation
– Quit Smoking: Smoking is a significant risk factor for many circulatory problems, including gangrene. Quitting smoking can improve blood flow and oxygenation to the tissues.
Monitor and Modify Environmental and Occupational Risks
1. Protective Clothing
– Appropriate Footwear: Wear properly fitting shoes to avoid injuries to the feet. This is particularly important for individuals with diabetes or peripheral neuropathy.
– Protect Against Extremes: Protect your extremities in extreme temperatures to prevent frostbite and heat injuries, which can lead to gangrene.
2. Safe Practices
– Avoid Constriction: Avoid wearing clothing or jewelry that is too tight, as it can restrict blood flow.
– Occupational Safety: If your job involves handling potentially harmful chemicals or operating heavy machinery, ensure that you use appropriate safety measures to prevent injuries.
Education and Awareness
1. Know the Signs
– Early Detection: Be aware of the early signs of gangrene, such as unexpected pain, numbness, skin discoloration, or foul odor from a wound.
– Educate Family and Caregivers: Inform those around you about what to watch for, especially if you have conditions that increase your risk.
2. Regular Medical Check-Ups: Regular health screenings can help catch and manage conditions that might lead to gangrene. Discuss with your doctor how often you should be examined based on your health status.
By implementing these prevention strategies, individuals can significantly reduce their risk of developing gangrene. It’s crucial for at-risk populations, especially those with diabetes or vascular diseases, to take proactive measures and seek timely medical advice to maintain optimal health and prevent complications.
Conclusion
Understanding the early signs of gangrene is fundamental for anyone at risk of this condition. With prompt detection and medical intervention, the outcomes can be significantly improved, and the severe consequences of gangrene can be averted. Always consult a healthcare provider if you notice any of the signs discussed, as early medical intervention is crucial.
FAQs
1. What is the most common type of gangrene?
2. How quickly does gangrene progress?
3. Can gangrene be treated without surgery?
4. What are the complications associated with untreated gangrene?
5. How can diabetics specifically prevent gangrene?
DR. ALOK KUMAR UDIYA
Well-known Interventional Radiologist Dr. ALOK KUMAR UDIYA is currently a consultant at The CARE CHL, an Indore hospital with NABH accreditation. He has a distinguished medical career and has studied at numerous top federal, state, and international superspecialty medical institutes.
He earned his M.B.B.S. from M G M Medical College in Indore and then M.D. in radiodiagnosis from Lady Hardinge Medical College at Delhi University.
Following that, he completed a fellowship in neuro- and vascular interventional radiology at the Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGIMS) in Lucknow, where he gained extensive experience in diagnostic imaging along with hepatobiliary, peripheral vascular, and neurovascular interventions.
The prestigious Institute of the liver and biliary sciences Hospital (ILBS), New Delhi, awarded him a P.D.C.C. (Post Doctoral fellowship) in Hepatobiliary intervention, where he also received further in-depth instruction and advanced training in hepatobiliary and transplant imaging and interventions.
Moreover, he completed a six-month Neuro-Interventional Fellowship (FINR) at the famous University of Zurich, where he received specialized training from Professor Anton Valavanis in the endovascular management of stroke and aneurysm. https://cvicvascular.com/
Contact Us
Contact No. – 099993 78980
Email – dralokudiya@gmail.com
Hospital
Care CHL
Address – AB Rd, near L.I.G Square, RSS Nagar, Indore, Madhya Pradesh 452008
Time – 10am to 5pm
Clinic
Address – 403 Panama Tower Geeta Bhawan Square Near Crown Palace, Indore, Madhya Pradesh
Time – 6pm To 8pm
Read More –
What is the main cause of peripheral vascular disease? – https://test.mangalcart.com/main-cause-of-peripheral-vascular-disease/
How do you diagnose peripheral artery disease? – https://test.mangalcart.com/diagnose-peripheral-artery-disease/
How do you treat a vascular disease? – https://test.mangalcart.com/how-do-you-treat-a-vascular-disease/