What is the main cause of peripheral vascular disease?
What is the Main Cause of Peripheral Vascular Disease?
Peripheral vascular disease (PVD), also known as peripheral artery disease (PAD), is a common circulatory problem in which narrowed arteries reduce blood flow to the limbs. Understanding the main causes of PVD is crucial for early diagnosis and effective management of the condition. This article delves into the primary cause, explores risk factors, and offers insights into prevention and management strategies for PVD.
Understanding Peripheral Vascular Disease
Peripheral vascular disease primarily affects the blood vessels outside of the heart and brain. The condition is often characterized by a narrowing of the vessels that carry blood to the legs, arms, stomach, or kidneys.
Peripheral Vascular Disease (PVD), also commonly referred to as Peripheral Artery Disease (PAD), involves disorders that cause the blood vessels outside of the heart and brain to narrow, block, or spasm. This can lead to reduced or blocked blood flow, most often in the arteries leading to the lower extremities.
The Physiology and Implications of PVD
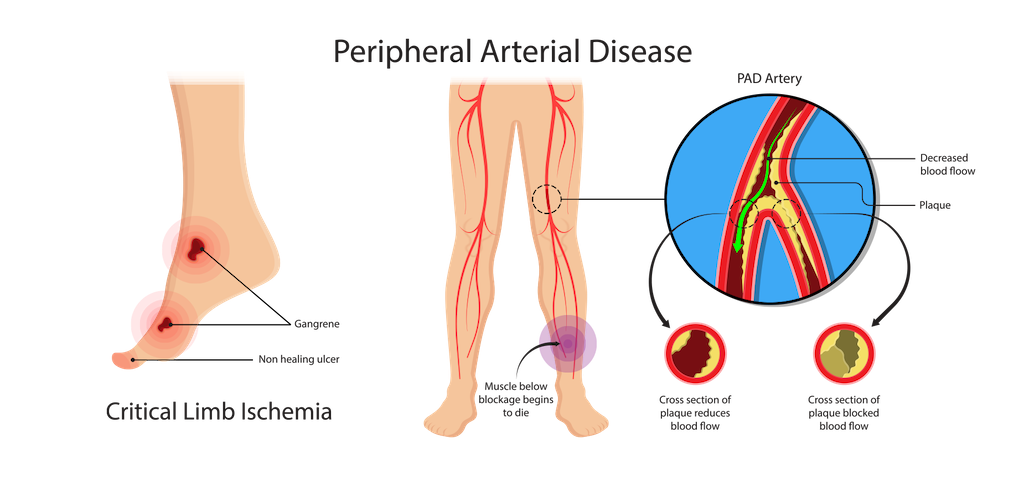
The primary physiological change in PVD is the narrowing of peripheral arteries due to atherosclerosis, where plaque builds up on the arterial walls. This plaque is mainly composed of fat, cholesterol, calcium, and other substances found in the blood. Over time, these deposits can harden and reduce the flexibility of the arteries, significantly diminishing blood flow.
Reduced blood flow can lead to several complications:
– Claudication: This symptom involves pain and cramping in the legs due to inadequate blood flow, especially during physical activities.
– Ischemia: Restricted blood flow can cause ischemia, which, if persistent, may lead to tissue damage and necrosis.
– Critical Limb Ischemia (CLI): In severe cases, the lack of blood flow can lead to the development of sores and wounds that do not heal, gangrene, and potentially the need for limb amputation.
Managing and Treating PVD
Management of PVD focuses on reducing symptoms and preventing progression of the disease. This can include:
– Lifestyle Changes: Quitting smoking, exercising regularly, and adopting a heart-healthy diet.
– Medications: Drugs to improve blood flow, manage symptoms, and treat underlying conditions such as high blood pressure and cholesterol.
– Surgical Procedures: In severe cases, procedures such as angioplasty, stenting, or bypass surgery may be required to restore adequate blood flow.
Understanding the complexity of Peripheral Vascular Disease is essential for managing the condition effectively. Early detection and proactive management can help mitigate the severe consequences associated with this disease, improving quality of life and reducing the risk of more severe complications like limb loss.
Atherosclerosis: The Leading Cause of PVD
Atherosclerosis is widely recognized as the principal cause of Peripheral Vascular Disease (PVD), a serious health condition affecting millions globally. This section delves into the mechanisms by which atherosclerosis leads to PVD, its implications, and strategies for management and prevention.
Mechanism of Atherosclerosis
Atherosclerosis begins with damage to the endothelium, the inner lining of the arteries. This damage can be triggered by various risk factors, including high cholesterol, high blood pressure, smoking, diabetes, and inflammatory processes often exacerbated by an unhealthy lifestyle. Once the endothelium is damaged, lipids from the blood can infiltrate the walls of the arteries, leading to the formation of plaques.
These plaques are made up of fats, cholesterol, calcium, and other substances from the bloodstream. Over time, these plaques grow and harden, which narrows the arteries and reduces the elasticity of the vessel walls—a process known as arteriosclerosis. As the artery lumen narrows, the blood flow to various parts of the body becomes restricted, leading to the symptoms and complications associated with PVD.
Impact of Atherosclerosis on Peripheral Arteries
The impact of atherosclerosis on peripheral arteries is significant because these arteries are crucial for supplying blood to the extremities. When plaque buildup narrows these arteries, it directly results in reduced blood flow to the legs and arms. This manifests clinically as claudication—pain and cramping in the affected limbs during activity—due to the muscles not receiving enough oxygen during exertion.
In more severe cases, the reduction in blood flow can lead to critical limb ischemia (CLI), characterized by severe pain at rest, non-healing ulcers, and gangrene. CLI is a serious condition that can result in limb amputation if not adequately addressed.
Understanding the relationship between atherosclerosis and PVD is essential for both patients and healthcare providers to effectively manage this condition. Early diagnosis and proactive management are key to preventing the severe consequences of this disease and maintaining a high quality of life.

Risk Factors Contributing to Atherosclerosis and PVD
Risk Factors Contributing to Atherosclerosis and PVD
Atherosclerosis, the underlying cause of Peripheral Vascular Disease (PVD), is a complex process influenced by a variety of risk factors. These risk factors can accelerate the progression of plaque buildup in the arteries, leading to narrowed or blocked arteries which can severely restrict blood flow. Understanding these risk factors is essential for the prevention and management of PVD. Here, we delve into the primary contributors that increase the likelihood of developing atherosclerosis and subsequently PVD.
1. Lifestyle Factors
– Smoking: Smoking is one of the most significant risk factors for atherosclerosis. It damages the lining of the arteries, increases arterial stiffness, raises blood pressure, and reduces the oxygen carrying capacity of the blood, which all contribute to the atherosclerotic process.
– Physical Inactivity: A sedentary lifestyle contributes to the development of atherosclerosis by exacerbating other risk factors such as obesity, high blood pressure, and diabetes.
– Unhealthy Diet: Diets high in saturated fats, trans fats, and cholesterol have been linked to the development of atherosclerosis. These fats contribute to the formation of plaque in the arteries.
2. Medical Conditions
– High Cholesterol Levels: High levels of low-density lipoprotein (LDL) cholesterol (“bad” cholesterol) and low levels of high-density lipoprotein (HDL) cholesterol (“good” cholesterol) can lead to the development of fatty deposits in the blood vessels, which can become atherosclerotic plaques.
– High Blood Pressure: Hypertension can cause damage to the artery walls, making them more susceptible to the accumulation of plaque.
– Diabetes: Diabetes significantly increases the risk of developing atherosclerosis. High blood sugar levels can damage the blood vessel lining and accelerate the growth of atherosclerotic plaque.
– Obesity: Excessive body weight is associated with higher LDL cholesterol levels, higher triglyceride levels, and higher blood pressure, all of which increase the risk of atherosclerosis.
3. Genetic Factors
– Family History: Genetics play a significant role in the development of atherosclerosis. Individuals with a family history of cardiovascular disease, including PVD, are at a higher risk of developing these conditions themselves.
4. Age and Gender
– Age: The risk of atherosclerosis increases with age due to the cumulative effects of exposure to other risk factors and the natural aging of the blood vessels.
– Gender: Men generally have a higher risk of developing atherosclerosis at a younger age compared to women. However, women’s risk increases and may surpass that of men post-menopause.
5. Inflammatory Processes
– Chronic Inflammation: Conditions characterized by chronic inflammation, such as lupus, rheumatoid arthritis, and chronic infections, can also contribute to the development of atherosclerosis. Inflammation plays a direct role in the atherosclerotic process by contributing to the formation and instability of plaques.
Addressing these risk factors not only helps in the prevention of PVD but also mitigates the risk of other cardiovascular diseases, promoting overall vascular health and longevity.

Symptoms and Diagnosis of PVD
Peripheral Vascular Disease (PVD), also known as Peripheral Artery Disease (PAD), is a common circulatory problem where reduced blood flow due to narrowed arteries leads to various symptoms, primarily in the legs. Recognizing the symptoms and obtaining an accurate diagnosis are crucial steps toward effective management of PVD.
Symptoms of Peripheral Vascular Disease
The symptoms of PVD can vary widely among individuals, and in some cases, the disease may be asymptomatic, particularly in the early stages. The most common symptoms include:
– Claudication: This refers to muscle pain or cramping in the legs or arms that starts during exercise and stops during rest. The pain is typically described as aching, cramping, or inducing fatigue, and it occurs due to inadequate blood flow during increased activity.
– Numbness or Weakness: Reduced blood flow can cause a feeling of numbness or weakness in the legs. This might also be accompanied by a noticeable decrease in temperature in one leg compared to the other.
– Change in Leg Color: As circulation diminishes, there might be noticeable changes in the color of the skin on the legs. The skin may appear paler or take on a bluish tinge.
– Slow Healing Sores: Sores or wounds on the toes, feet, or legs that heal slowly or not at all can be a sign of PVD. This is due to insufficient blood flow needed for healing and tissue repair.
– Hair Loss or Slower Hair Growth: The legs and feet might experience hair loss or reduced hair growth as a result of decreased blood flow.
– Shiny Skin on the Legs: The skin on the legs may look shiny and tight, suggesting changes in the skin due to blood flow issues.
– Pulse Changes in the Legs: The pulses in the feet and legs may become weaker, to the point where they are difficult to detect.
Diagnosis of Peripheral Vascular Disease
Diagnosing PVD involves several steps, typically starting with a review of the patient’s medical history and a physical examination. Key diagnostic tests include:
– Physical Examination: The doctor will look for physical signs of PVD, such as weak or absent pulses in the extremities, reduced blood pressure in the affected limb, or any changes in the appearance of the feet and legs.
– Ankle-Brachial Index (ABI): This simple, non-invasive test compares the blood pressure measured at the ankle with the blood pressure measured at the arm. An ABI ratio of less than 0.9 usually indicates PVD.
– Doppler and Ultrasound Imaging: These imaging tests visualize blood flow in the veins and arteries using high-frequency sound waves. They can show blockages or narrowing of the arteries.
– Angiography: By injecting a contrast agent into the body and taking X-rays, angiography allows for detailed visualization of the blood vessels. This can help identify specific locations and severity of artery narrowing.
– Magnetic Resonance Angiography (MRA) and CT Angiography: These tests provide high-resolution images of the arteries and can show both the blood flow and the structure of the blood vessels.
Prompt diagnosis is essential as PVD can lead to more serious complications, including critical limb ischemia and increased risk of heart attack and stroke. Early diagnosis allows for earlier intervention and better management of the condition to prevent its progression. Lifestyle changes, medications, or in some cases, surgical interventions can significantly improve the quality of life for those affected by PVD.
Prevention and Management of PVD
Preventing and managing Peripheral Vascular Disease (PVD) involves a combination of lifestyle modifications, medical treatments, and in some cases, surgical interventions. The goals are to stop the progression of the disease, alleviate symptoms, improve mobility and quality of life, and reduce the risk of complications such as heart attack, stroke, and limb amputation.
Preventive Measures
Prevention is key in the management of PVD, particularly for individuals at higher risk due to underlying conditions like diabetes, hypertension, or hyperlipidemia. Here are effective strategies to prevent the onset or progression of PVD:
– Quit Smoking: Smoking cessation is crucial, as smoking is a major risk factor for the development and worsening of PVD. Quitting smoking can halt further damage to the arterial walls.
– Regular Physical Activity: Exercise helps improve circulation and heart health, which can prevent the symptoms of PVD from worsening. Walking, cycling, and swimming are excellent forms of aerobic exercise that help condition the muscles to use oxygen more efficiently.
– Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce blood pressure, cholesterol levels, and body weight—all risk factors for PVD.
– Weight Management: Maintaining a healthy weight reduces the burden on the circulatory system and decreases the risk of diabetes and hypertension.
– Manage Blood Sugar Levels: For individuals with diabetes, controlling blood sugar levels is critical to prevent the progression of PVD.
– Regular Health Screenings: Frequent monitoring of blood pressure, cholesterol, and blood sugar levels can help catch and address changes that may indicate an increased risk of PVD.
Management of PVD
Once PVD is diagnosed, management focuses on reducing symptoms and preventing the disease from worsening. The management plan may include:
Medications:
– Antiplatelet agents such as aspirin or clopidogrel to prevent blood clots.
– Cholesterol-lowering drugs (statins) to reduce cholesterol levels and stabilize plaques in the arteries.
– Blood pressure medications to control hypertension.
– Medications for diabetes management to control blood sugar levels.
– Cilostazol or Pentoxifylline to improve symptoms of claudication.
Supervised Exercise Therapy: A structured exercise program supervised by a healthcare professional can significantly improve walking distance and speed for individuals with claudication.
Foot Care: Proper foot care is essential for people with PVD to prevent sores and infections that can lead to serious complications. This includes regular inspection of the feet, wearing appropriate footwear, and keeping the feet clean and moisturized.
Surgical Treatments
For severe cases of PVD where lifestyle changes and medications do not sufficiently alleviate symptoms, surgical options may be considered:
– Angioplasty and Stent Placement: This procedure involves inserting a balloon to expand the narrowed artery, often followed by placing a stent to keep the artery open.
– Bypass Surgery: This involves using a vessel from another part of the body or a synthetic tube to bypass the blocked artery, allowing blood to flow around the narrowed or blocked section.
– Atherectomy: This is a procedure to remove plaque from the arteries.
Ongoing Monitoring and Care
Regular follow-ups with healthcare providers are essential for monitoring the progress of treatment, making necessary adjustments, and ensuring optimal management of the condition. Education about the disease and its management is also crucial for patient compliance and improvement.
Effective prevention and management of PVD are pivotal in mitigating its impact on health and lifestyle. By adopting a proactive approach in addressing risk factors and symptoms, individuals with PVD can lead healthier and more active lives.
Conclusion
The main cause of peripheral vascular disease is atherosclerosis, a condition marked by the buildup of plaque in the arteries. Understanding the risk factors and symptoms associated with this disease is essential for effective management and prevention. By adopting a healthy lifestyle and managing risk factors, individuals can significantly reduce their chances of developing PVD.
FAQs
1. How does smoking affect peripheral vascular disease?
2. What are the best exercises for someone with peripheral vascular disease?
3. What diet changes can help manage or prevent PVD?
4. How often should someone at risk of PVD see a doctor?
5. What are the latest treatments for PVD?
6. How can I tell if I have PVD or another condition like neuropathy?
DR. ALOK KUMAR UDIYA
Well-known Interventional Radiologist Dr. ALOK KUMAR UDIYA is currently a consultant at The CARE CHL, an Indore hospital with NABH accreditation. He has a distinguished medical career and has studied at numerous top federal, state, and international superspecialty medical institutes.
He earned his M.B.B.S. from M G M Medical College in Indore and then M.D. in radiodiagnosis from Lady Hardinge Medical College at Delhi University.
Following that, he completed a fellowship in neuro- and vascular interventional radiology at the Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGIMS) in Lucknow, where he gained extensive experience in diagnostic imaging along with hepatobiliary, peripheral vascular, and neurovascular interventions.
The prestigious Institute of the liver and biliary sciences Hospital (ILBS), New Delhi, awarded him a P.D.C.C. (Post Doctoral fellowship) in Hepatobiliary intervention, where he also received further in-depth instruction and advanced training in hepatobiliary and transplant imaging and interventions.
Moreover, he completed a six-month Neuro-Interventional Fellowship (FINR) at the famous University of Zurich, where he received specialized training from Professor Anton Valavanis in the endovascular management of stroke and aneurysm. https://cvicvascular.com/
Contact Us
Contact No. – 099993 78980
Email – dralokudiya@gmail.com
Hospital
Care CHL
Address – AB Rd, near L.I.G Square, RSS Nagar, Indore, Madhya Pradesh 452008
Time – 10am to 5pm
Clinic
Address – 403 Panama Tower Geeta Bhawan Square Near Crown Palace, Indore, Madhya Pradesh
Time – 6pm To 8pm
Read More –
Carotid Stenting – https://test.mangalcart.com/carotid-stenting/
What Does Early Signs of Gangrene Look Like? – https://test.mangalcart.com/what-does-early-signs-of-gangrene-look-like/
What is the cost of AVM embolization in India? – https://test.mangalcart.com/cost-of-avm-embolization-in-india/
